Generic Medications: What They Are, How They Work, and Why They Matter
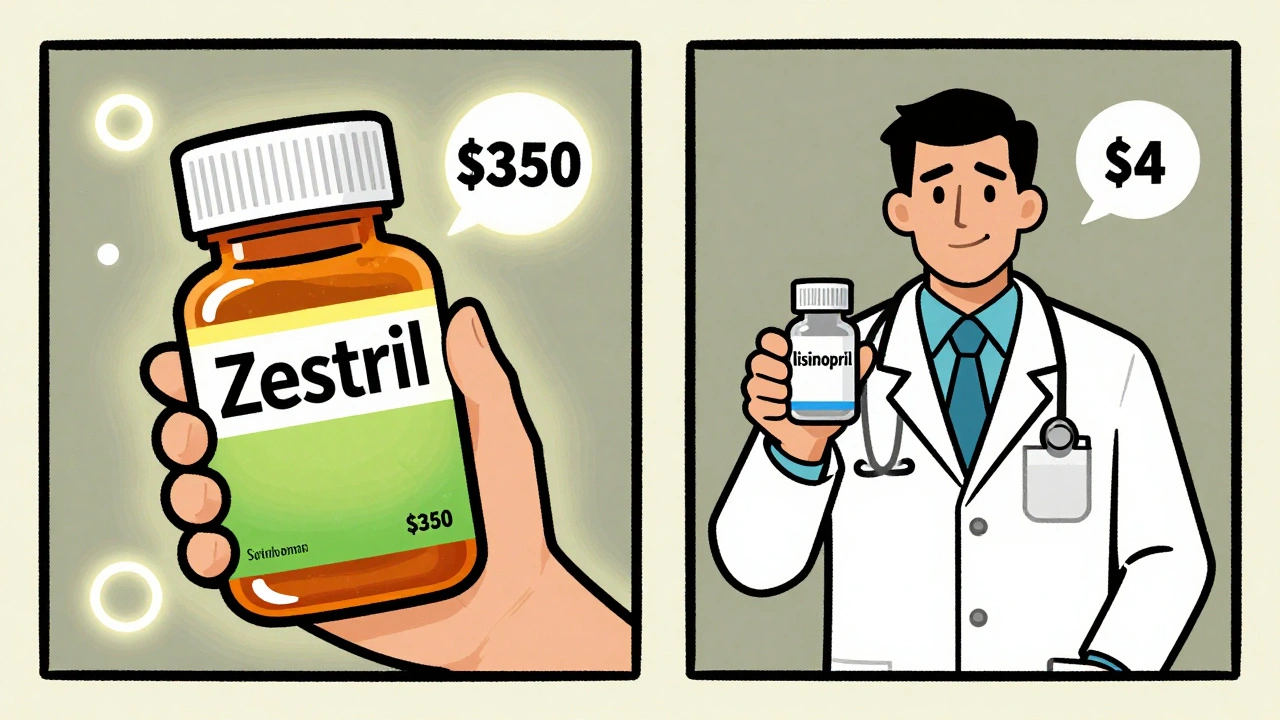
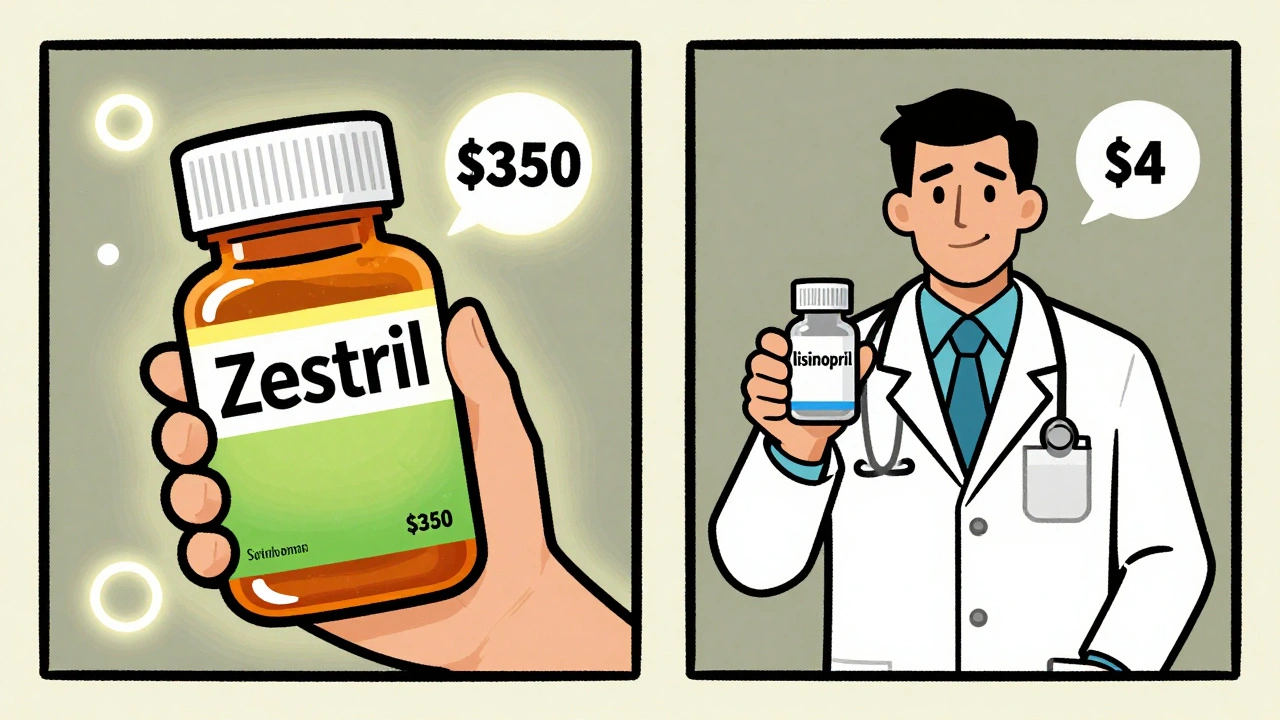
When you hear generic medications, pharmaceutical products that contain the same active ingredients as brand-name drugs but are sold under their chemical name. Also known as generic drug alternatives, they work the same way, in the same dose, and with the same risks and benefits as the original—just for a fraction of the price. Most people assume generics are cheaper because they’re lower quality, but that’s not true. The FDA requires them to meet the same strict standards for strength, purity, and performance as brand-name drugs. The only differences? The color, shape, flavor, or inactive ingredients—and the price tag, which can be 80% to 95% lower.
Why does this matter? Because authorized generics, exact copies of brand-name drugs made by the original manufacturer and sold under a generic label are often the closest thing to the original you can get—same factory, same formula, same packaging, just cheaper. But not all generics are created equal. Some are made by foreign labs with inconsistent quality control, and others get approved without full bioequivalence testing. That’s why knowing where your meds come from, and how they’re tested, can make a real difference in how you feel.
Drug substitution, when a pharmacist swaps a brand-name drug for a generic without asking your doctor is legal in most places—but not always safe. In some states, pharmacists can switch your medication automatically, even if your doctor wrote "dispense as written." And if you’re on something like levothyroxine or warfarin, even tiny changes in absorption can throw off your whole treatment. That’s why understanding your rights, your insurer’s formularies, lists of approved drugs that determine what your insurance will pay for, and how to ask for the right version matters more than you think.
Insurers push generics because they cut costs—and that’s good for you if you’re paying out of pocket. But they also control what you get. If your formulary lists only one generic version of a drug, and you react poorly to it, you might be stuck until your doctor fights back. Meanwhile, some patients end up switching between different generic brands every few months, wondering why their symptoms keep changing. It’s not your imagination. Different fillers, binders, and coatings can affect how your body absorbs the medicine.
And here’s the thing: most people don’t realize that the same generic drug can be made by ten different companies, each with their own quality control. One batch might work perfectly. Another might leave you dizzy or nauseous. That’s why knowing how to read your prescription, ask your pharmacist about the manufacturer, and check the FDA’s list of authorized generics can save you from unnecessary side effects.
There’s no magic to generics. They’re not second-rate. They’re just smart. But like any tool, they need to be used right. Whether you’re managing thyroid levels, blood pressure, or depression, the right generic can keep you stable and save you hundreds a year. The wrong one? It could cost you more in doctor visits, ER trips, and lost days at work.
Below, you’ll find real, practical guides on how to spot the good from the bad, when to push back on substitutions, how to read FDA reports, and what to do if your insurance won’t cover the version your body needs. No fluff. No theory. Just what works—for your health, your wallet, and your peace of mind.

Spanish-language resources help patients understand that generic medications are just as effective as brand-name drugs - and much cheaper. Learn where to find trusted tools, common misunderstandings, and how to use them safely.
Continue Reading
Generics work just as well as brand-name drugs - and save patients up to 90% on costs. Yet many doctors still prescribe brands, and patients refuse generics. Here’s why - and how to overcome the psychology behind the resistance.
Continue Reading